Our research is changing the world for the better and improving the health of people locally, nationally and globally.
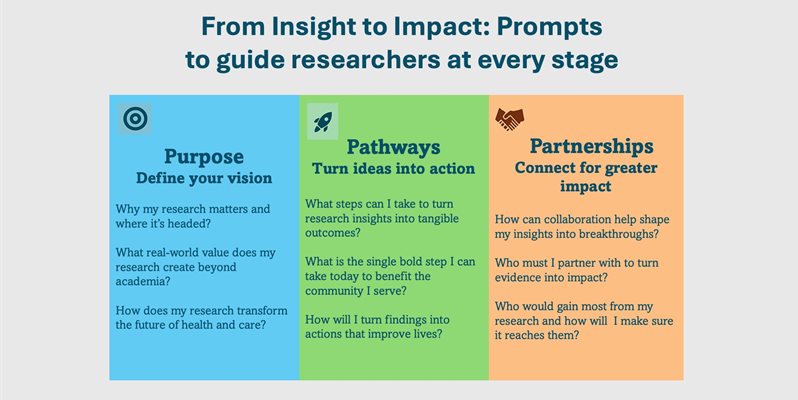
At BSMS, we are dedicated to fostering a strong culture of research impact. In recent years, we have invested in enhancing our impact culture with an emphasis on building capacity and supporting researchers at every career stage. From the outset, we encourage researchers to embed impact into their work through “stakeholder” engagement, impact planning, and aligning objectives with real-world needs. To guide this process, we also invite researchers to reflect on a series of impact prompts such as:
Our research is driving real-world change shaping clinical guidelines, improving quality of life for individuals affected by liver disease, cancer, HIV, scabies, podoconiosis, and more; reducing youth smoking; and informing both national and global health and sustainability policies. We are tackling urgent challenges in health, wellbeing, and care to benefit communities locally, nationally, and internationally.
The stories we share here highlight the breadth and depth of our impact, showcasing how our recent and ongoing projects are transforming healthcare, influencing policy and practice, and reaching diverse populations at every level.
Brighton and Sussex Medical School

Emerging Impact
Controlling institutional scabies outbreaks in care homes for the elderly, refugee camps, and beyond

EMERGING IMPACT
Using computer simulations of blood cancer to tailor treatment

ref impact case study
Turning the tide on the awareness, treatment and prevention of podoconiosis
EMERGING IMPACT
Engaging with patients and the public about new genomic medicine technologies through creative methods

REF IMPACT CASE STUDY
How we are working with rough sleepers and people who use drugs to eliminate hepatitus C virus

EMERGING IMPACT
Palliative care in advanced chronic liver disease: time for action

REF IMPACT CASE STUDY
Transforming the management of hypertension in the over 80s group

EMERGING IMPACT
Time for Dementia: enhancing dementia care in the future healthcare workforce

REF IMPACT CASE STUDY
Enabling a more rational approach to antibiotic prescribing and usage
EMERGING IMPACT
Improving healthcare experiences for neurodivergent people

REF IMPACT CASE STUDY
Delayed umbilical cord clamping: a ray of hope for improved survival and better health outcomes for premature babies

REF IMPACT case study
Asthma: personalised clinical care improves treatment and management

REF IMPACT CASE STUDY
Patient' preferences for different methods of delivering trastuzumab in treatment of her2-positive breast cancer

EMERGING IMPACT
A new way of managing children’s allergy and asthma

EMERGING IMPACT
Paradigm change for trials and treatment in ALS

EMERGING IMPACT
Developing sustainable models of high-quality healthcare

Emerging impact
HIV and STI diagnosis and treatment
Emerging impact
Emerging Innovations in Infection Prevention: Shaping the Future of Global Health

Emerging impact
Evaluating the impact of tobacco control policies

Emerging impact
Implementation preferences for the management of STIs
Emerging Impact
Consultation, Campaign and Medication: Changing public understanding of scabies

Emerging impact
Building the dementia workforce of the future

Emerging impact
Elevated blood pressure and hypertension

Emerging impact
Long-acting HIV treatment included in WHO treatment guidelines

REF IMPACT case study
Integrating medicine, conservation and climate action in Papua New Guinea’s rainforests

EMERGING IMPACT
Uncovering the immune mechanisms behind podoconiosis

REF IMPACT CASE STUDY
Reducing alcohol-related harm through “Dry January”

EMERGING IMPACT
Advancing Tuberculous Meningitis Treatment in LMICs

Emerging impact
Laying the Foundations for Community-Led Hearing Care
Box heading - text only
Box strapline - text only
Button link - add button-link-white class to link
BACKGROUND IMAGE FOR PANEL
BACKGROUND IMAGE FOR PANEL
Asthma: personalised clinical care improves treatment and management

Asthma is a common medical condition affecting the breathing of both children and adults, which can have a life-long negative impact on quality of life. The research led by Professor Somnath Mukhopadhyay (view his profile here) is helping to transform the management of asthma and allergy, change treatment practice and improve patient outcomes.
By developing personalised medicine clinics, which explore specific genetics, allergic traits and other individual characteristics to provide tailored care, the work of Professor Mukhopadhyay and colleagues has enabled the provision of holistic care to children. These clinics are now a standard practice at the Royal Alexandra Children’s Hospital, Brighton.
This work has changed patients’, parents’ and clinicians’ perceptions of asthma treatment plans, while also generating new understanding of the role of genetic variation in delivering tailored care, thus improving children’s overall quality of life and experience. In addition, using this individualised approach has helped clinicians gain parents’ trust as they feel understood and heard, making the work more meaningful.
Reviewing childhood asthma deaths in New South Wales, the Medical Journal of Australia commented that Mukhopadhyay’s work might explain the reduced response to asthma medicines and consequent deterioration and death in some children, possibly as a result of their underlying adverse gene status. Thus, a distinct highlight of Mukhopadhyay’s work is that it has informed healthcare practitioners in Australia and the findings of his research influenced subsequent prescribing advice in the Asthma Australia Handbook (2015). Hence, the impact of this research has extended globally, beyond clinical applications within the NHS.
Through participation in the Brighton Fringe Festival (2016), British Science Festival (2017) and New Scientist Science Forum (2018), the work has raised public awareness of and encouraged discussion on personalised medicine for asthma. The findings were received with great interest when presented to pupils and staff in schools in Portugal and West Bengal (India) and resulted in greater awareness and understanding of how asthma and allergy may affect each child in a different manner and how personalised management approaches may thus result in more holistic care for children with asthma.
This work has attracted funding from Action Medical Research and the Henry Smith Charity, both known for bringing a positive change to personalised health care research.
Read more about our paediatric research here >
Turning the tide on the awareness, treatment and prevention of podoconiosis
 Have you heard of podoconiosis? Do you know where it is found or how it is caused? Professor Gail Davey, together with Dr Kebede Deribe, Professor Melanie Newport and colleagues, have been working to understand the extent of the problem and have helped to implement measures designed to raise awareness, reduce stigmatisation and improve the treatment of podoconiosis. Podoconiosis is a debilitating disease which causes swelling of the feet and legs. It is common in tropical areas, particularly in Africa, Central and South America, and Southeast Asia. It disproportionally affects the poorest people, in farming households, who work barefoot and are exposed to irritant red clay soil of volcanic origin. Those affected experience disabling consequences such as weeping swollen feet, which impacts their ability to earn a livelihood, often leading to depression and inability to care for their families. In addition, the disease brings stigma and exclusion. The team led by Professor Davey, has been focussing largely on Ethiopia and Rwanda, where podoconiosis is particularly prevalent. Their studies have brought in experts from genetics, ethics, law, mineralogy, biochemistry and geology. This multidisciplinary approach led to an increased awareness and understanding of this disease both locally and at the level of national government. This pioneering research has attracted implementation funding from the UK Big Lottery Fund and IZUMI Foundation. Much has changed since this programme of research commenced in 2002. It has drawn the attention of policymakers such that podoconiosis is one of the nine Neglected Tropical Diseases (NTD) prioritised in Ethiopia. What’s more, it has shed new light on how the role of simple treatment interventions such as foot washing, skin care, exercise, elevation, and the use of socks and shoes are effective in reducing the impact of this disease. This research has fed into key reports and policy documents, including the Rwanda NTD Master Plan (2019-2024) and in the Ethiopia NTD Master Plan (2020-2025). This research is helping improve our collective knowledge about the disease that has remained neglected for so long. The ongoing work and its impact on patients, health workers and policy makers give hope that the disease can be eliminated within our lifetime.Read more about our podoconiosis research here >
Have you heard of podoconiosis? Do you know where it is found or how it is caused? Professor Gail Davey, together with Dr Kebede Deribe, Professor Melanie Newport and colleagues, have been working to understand the extent of the problem and have helped to implement measures designed to raise awareness, reduce stigmatisation and improve the treatment of podoconiosis. Podoconiosis is a debilitating disease which causes swelling of the feet and legs. It is common in tropical areas, particularly in Africa, Central and South America, and Southeast Asia. It disproportionally affects the poorest people, in farming households, who work barefoot and are exposed to irritant red clay soil of volcanic origin. Those affected experience disabling consequences such as weeping swollen feet, which impacts their ability to earn a livelihood, often leading to depression and inability to care for their families. In addition, the disease brings stigma and exclusion. The team led by Professor Davey, has been focussing largely on Ethiopia and Rwanda, where podoconiosis is particularly prevalent. Their studies have brought in experts from genetics, ethics, law, mineralogy, biochemistry and geology. This multidisciplinary approach led to an increased awareness and understanding of this disease both locally and at the level of national government. This pioneering research has attracted implementation funding from the UK Big Lottery Fund and IZUMI Foundation. Much has changed since this programme of research commenced in 2002. It has drawn the attention of policymakers such that podoconiosis is one of the nine Neglected Tropical Diseases (NTD) prioritised in Ethiopia. What’s more, it has shed new light on how the role of simple treatment interventions such as foot washing, skin care, exercise, elevation, and the use of socks and shoes are effective in reducing the impact of this disease. This research has fed into key reports and policy documents, including the Rwanda NTD Master Plan (2019-2024) and in the Ethiopia NTD Master Plan (2020-2025). This research is helping improve our collective knowledge about the disease that has remained neglected for so long. The ongoing work and its impact on patients, health workers and policy makers give hope that the disease can be eliminated within our lifetime.Read more about our podoconiosis research here >
BACKGROUND IMAGE FOR PANEL
How we are working with rough sleepers and people who use drugs to eliminate hepatitis C virus

According to data from the homeless charity Shelter (2021), Brighton and Hove has one of the highest rates of homelessness in the UK, after London and Luton. Homelessness exposes individuals to many vulnerabilities such as poor health, unemployment and depression. In addition, alcohol and drug dependence can be very high amongst rough sleepers, thus increasing their exposure to infectious diseases such as hepatitis C virus (HCV) and HIV.
Over the past decade, Professor Sumita Verma (view her profile here) and her team have reached out to these hard-to-reach, high-risk, populations to provide HCV treatment. HCV affects the liver and can lead to serious liver disease if left untreated.
A unique aspect of this research is that the team chose to work in the community setting unlike the traditional hospital- based care. They used a ‘one-stop’ care model that included screening of people who use drugs and homeless individuals at the Brighton Pavilion, one of the largest addiction centres. A community-based nurse offered treatment and a painless liver scan to assess for liver scarring. Addiction teams, peer mentors and social workers joined in to ensure effective care and delivery of service. The work gradually expanded into Arch Healthcare, the only surgery in Brighton and Hove, providing specialised healthcare to people experiencing homelessness or using hostel services.
The response to this community-based HCV service has been overwhelmingly positive. Patients really valued the personal, flexible, engaging, and non-judgemental approach, far more than going through hurdles to access care in hospitals. Cure rates have been comparable to hospital- based treatment. Deaths from hepatitis C virus related liver disease almost halved in Brighton, though other factors also contributed to this. This work also had a significant positive impact on the individual’s quality of life and understanding of their disease and their ability to access treatment. As a result, once the HCV was treated, many were able to address other issues in their lives such as their drug or alcohol use.
This research has changed the way patients, GPs, nurses, social workers perceive people who use drugs and rough sleepers and their associated health issues. The new HCV care model developed by Professor Verma and team has been rolled out in other UK centres, which shows the breadth and impact of their work. Their research-led interventions are playing a vital role in achieving the national goal of eliminating HCV by 2025; adoption of some of these interventions has enabled two of the largest HCV centres to achieve NHS England HCV elimination targets. Furthermore, Professor Verma has secured further funding from a leading international pharmaceutical company, Gilead Sciences to develop similar care models throughout East and West Sussex.
This study has shone a light on some of the health inequalities that exist in marginalised communities in the UK. The work of Professor Verma and team and translated into a positive treatment and care experience in the lives of those enduring drug use, homelessness, poverty and ill health.
BACKGROUND IMAGE FOR PANEL
Transforming the management of hypertension in the over 80s age group

High blood pressure (hypertension) is a prevalent condition in the elderly, which can lead to serious health risks such as heart attack and stroke. While several research studies had been conducted on the treatment and management of hypertension, very few have focused on the very elderly, people aged 80 years and over. Indeed, this group had been largely overlooked and under-studied in public health.
Research undertaken by Professor Rajkumar Chakravarthi (view his profile here) and colleagues over the last two decades has addressed this gap, through the international HYVET Trial (Hypertension in the very elderly trial). This trial was the first large trial of blood pressure-lowering treatment in the very elderly. The trial recruited 3845 participants across 195 centres in 13 countries in Europe, China, Australasia and North Africa. The trial set a target blood pressure threshold of under 150/90 mm/Hg to manage hypertension. Participants were prescribed the diuretic drug indapamide and the ACE inhibitor perindopril to achieve blood pressure below the target threshold.
Working collaboratively with the British Heart Foundation and the Institut de Recherches Internationales Servier, the trial achieved some important outcomes. Two years into the treatment, 80% of patients successfully met the blood pressure target, which was associated with a 30% reduction in the rate of fatal or non-fatal stroke; a 21% reduction in the rate of death from any cause; a 23% reduction in the rate of death from heart and circulatory events; and a 64% reduction in the rate of heart failure. The success of this ground-breaking trial led to its incorporation into NICE clinical guidelines in the UK and wider adoption of its findings internationally.
This research represents a significant advancement in the quality of care of the population aged over 80 with hypertension. It has changed clinical practice and significantly improved health outcomes among those aged 80 and over with hypertension. What is more, the research confirms the importance of delivering appropriate healthcare for the very elderly.
Enabling a more rational approach to antibiotic prescribing and usage

Have you been prescribed antibiotics to treat a bacterial infection? Were you asked to complete the course and warned not to stop the treatment early?
Antibiotics are some of the most commonly prescribed medicines in the UK but excessive or unnecessary use of antibiotics is leading to the emergence of new antibiotic resistant infections. This is reducing the effectiveness of antibiotics for current and future patients.
Professor Martin Llewelyn (view his profile here) and colleagues found that the ‘Start Smart then Focus’ initiative, led by Department of Health, designed to review and revise hospital patients’ prescriptions is not implemented effectively in NHS hospitals. To address this pressing issue, his team developed the Antibiotic Review Kit (ARK) programme, an intervention to review and revise patients’ prescriptions within 24-72 hours with the aim of safely stopping or reducing the use of antibiotics based on clinical evidence. A key aspect of the work was challenging the dogma that stopping antibiotics earlier than dictated by traditional course-lengths increases rather than decreases resistance.
Since its implementation, the ARK programme has had a tangible impact in changing the way both patients and front-line hospital staff perceive antibiotics dosage and effectiveness. It has empowered junior doctors, pharmacists, consultants and health care workers to, stop unnecessary use of antibiotics and make a difference to patients’ treatment. When introduced at the Trust, the antibiotic stop rate increased from 9 per cent to 36 per cent with no associated adverse outcomes.
Since then, the intervention has been implemented in 40 ARK acute NHS trust from all four nations of the UK. Overall, the ARK intervention was associated with sustained reductions in antibiotic use of 4% year on year compared with the NHS target of 1% without evidence of patient harm. Furthermore, one of the leading providers of electronic prescribing systems to NHS hospitals (Wellsky) had implemented the AKR prescription approach into its antibiotic prescribing module.
A unique aspect of this research is that the tools it has developed to support prescribers are now freely available and ready for adoption through a collaboration with the British Society for Antimicrobial Chemotherapy. The learning module and all associated materials can be accessed with registration here:
Through evidence-based training, observational and behavioural interventions, the work of Professor Llewelyn and colleagues has provided a framework for rational antibiotic prescribing and evaluation of continued usage. This approach should help to reduce unnecessary antibiotic usage and prevent the emergence of antibiotic resistant bacteria.
BACKGROUND IMAGE FOR PANEL
Delayed umbilical cord clamping: a ray of hope for improved survival and better health outcomes for premature babies

Premature birth is one of the leading causes of death in babies and children up to the age of five. Early clamping of the umbilical cord, a traditionally standard practice, has been associated with neonatal complications, particularly in premature babies.
Research led by Professor Heike Rabe (view her profile here) on delayed cord clamping (DCC) has contributed to improved outcomes and health benefits, including reduced risk of premature deaths and increased survival rates among infants. A delay in clamping of at least 30 seconds and up to 3 minutes can enhance redistribution of placental blood in the baby, stabilise blood pressure, reduce brain haemorrhage and lower rates of anaemia. It can also contribute to better overall care outcomes for complex premature births.
This impactful research on DCC has been instrumental in shaping wider public health strategies to improve both infant and maternal health. It has directly influenced and informed 17 national and international clinical guidelines, including the WHO Care of the Newborn Infant and NICE Preterm Labour and Birth guidelines. Consequently, there has been a shift in understanding, acceptance and practice of DCC in preterm births in the EU, Canada and USA.
An important feature emerging from this research is the development of British Association of Perinatal Medicine Optimal Cord Management Toolkit. It has been implemented in maternity and neonatal units across NHS England, which has contributed to the frequency of DCC rising from 30 to 85 per cent in preterm births in one year in West and South West England. See more here.
A unique feature of this research is that it has contributed to translating scientific evidence into teaching sessions for health care practitioners. The midwifery team and junior medical staff within the NHS attend DCC sessions as part of their induction and mandatory study days. Furthermore, this research is being publicly acknowledged, shaping conversations on awareness of among consumer organisations, professional bodies, guideline developers and policy makers.
Professor Rabe’s work has strengthened the evidence base supporting the routine adoption of DCC. This is seemingly minor change in clinical practice is giving premature infants the best opportunity to thrive during the crucial first few weeks of life.
BACKGROUND IMAGE FOR PANEL
Patients’ preferences for different methods of delivering trastuzumab in the treatment of HER2-positive breast cancer

Almost one in five breast cancers are HER2-positive. It can be treated successfully with a drug called trastuzumab which was usually given intravenously (an infusion into a vein). This treatment poses several challenges; patients who have completed their surgery and chemotherapy are required to continue attending hospital for trastuzumab infusions once every three weeks for 12 months. Setting up IV infusions and delivering the drug could sometimes take several hours and patients had to travel to cancer centres. This can be enormously burdensome for patients who just wish to resume everyday life as it involves such a significant amount their time. It is also costly and time-consuming for chemotherapy departments. A new method of administering the drug through a subcutaneous injection (under the skin) taking just five minutes was developed and research studies showed that it was safe to administer the drug in this way. An international study was then launched to find out which method of delivery patients preferred and why.
In 2011, Professor Dame Lesley Fallowfield (view her profile here) and colleagues at the Sussex Health Outcomes Research and Education in Cancer Centre (SHORE-C) led the research finding out which system of delivery, intravenous or subcutaneous, patients preferred and reasons why. This was a large, randomised study, called PrefHER, conducted in 10 European countries, Turkey and Canada. A computer randomly sorted HER2- positive patients into 2 groups – Group 1) received SC treatment every three weeks for four months then crossed over to IV delivery Group 2) received IV treatment every three weeks for four months then crossed over to SC delivery. Before starting treatment, patients were interviewed in their own languages by specially trained interviewers about issues such as their attitudes to needle and injections. At the end of study treatment patients completed further interviews regarding their experiences and preferences.
A challenging aspect of this study was the need for a multilingual approach. SHORE-C had to produce educational DVDs in 10 different languages explaining the study and a comprehensive manual for the use of all interviewers. which aided their ability to develop trust and rapport with the patients. Training DVDs were also produced for the healthcare professionals who were delivering trastuzumab subcutaneously.
The PrefHer study showed that patients had a strong and compelling preference for SC delivery as it saved so much time, caused less pain and discomfort and was more convenient then IV administration.
This research, led by Professor Dame Lesley Fallowfield contributed to the approval by NICE in the UK and health authorities in other countries of SC delivery of trastuzumab. The approach also offers the potential for treatment closer to patient’s home – a central tenet of the NHS Five Year Forward plan for improvement in health outcomes for cancer patients.
Read more about SHORE-C here >
Integrating medicine, conservation, and climate action in Papua New Guinea’s rainforests
The island of New Guinea contains earth’s third largest remaining tropical rainforest, home to myriad human cultures and a huge abundance of species. However, this rainforest, and the bio-cultural diversity it protects, are threatened by commercial logging driven primarily by global commodity demands, and its mostly rural population face difficulties accessing medical services.
In response to these intersecting crises, Jo Middleton (Research Fellow in Primary Care and Public Health) and friends have established deep in the forest a permanent clinic (pictured above) serving previously medically neglected communities across 500 square kilometres. As well as improving community health, this is protecting 15,000 hectares of highly biodiverse rainforest, storing 1.5 million tonnes of carbon.
In 2018, Jo led a team from BSMS and New Guinea Binatang Research Centre which responded to a request from clans who had defended their rainforest from loggers, but lacked access to biomedicine. They treated urgent cases and conducted a needs assessment to co-plan with the community how to incorporate health services into their indigenous-led conservation alliance. Jo then worked with ecologists Alan Stewart and Mika Peck (Life Sciences, Sussex) to use the study results to successfully win UK government aid funding to establish primary care in support of Wanang’s forest preservation.
Enacting a three-phase health plan based on the study findings, Jo returned in 2019 to carry out phase one which involved training a community emergency response and evacuation team. In phase two, they returned again in 2020 to support the building and opening of a nurse-staffed clinic. In the third ongoing phase, the clinic is being used by Jo and colleagues as a base for health patrols in surrounding communities, targeting high priority burdens such as tropical skin diseases and malaria.
As well as supporting conservation at Wanang, this work encouraged neighbouring clans that previously chose to allow logging to join the conservation area, expanding it in size by fifty percent. In addition, the forest itself is acting as a natural laboratory for ecological studies, with community members trained to carry out fieldwork, bringing valuable income to local families.
The project’s successful conservation and clinical outcomes have inspired similar action elsewhere in the country, and as far afield as Ecuador. The impacts of this multidisciplinary action-research highlight a fresh approach to promoting conservation, health, and climate action through meaningful engagement with, and the active involvement of, local indigenous communities.
Read more about the project here >
BACKGROUND IMAGE FOR PANEL
Reducing alcohol-related harm through “Dry January”

BSMS research led by Professor Richard de Visser has played a major role in shaping and expanding the global “Dry January” movement – helping thousands of people to drink less, feel healthier, and stay in control of their drinking.
Professor de Visser’s studies explored how taking part in a month-long alcohol break influences health, wellbeing, and longer-term drinking habits. His findings showed that people who complete Dry January report better sleep, improved concentration, more energy, and financial savings. Six months later, many report drinking less and feel more confident managing their alcohol use.
The research also demonstrated that using structured support – such as official sign-up tools and motivational messages – doubles the likelihood of successfully completing the challenge. These insights directly informed Alcohol Change UK’s approach to promoting Dry January and developing its resources for participants.
Beyond the UK, the research inspired the creation of “Dry January à la française”, launched in 2020. French health leaders described the BSMS research as “critical” in bringing national organisations together to start the campaign.
Through this work, Professor de Visser’s research has contributed to improving public health, reducing alcohol-related harm and empowering people to make positive lifestyle changes across the UK and beyond.
The full Impact Case Study (including references) is available below.
Read the full impact case study >
BACKGROUND IMAGE FOR PANEL
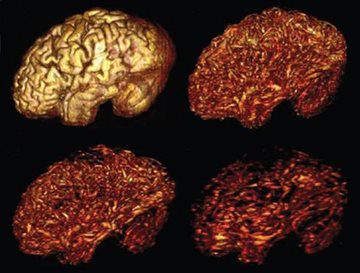
Using computer simulations of blood cancer to tailor treatment

As we learn more about blood cancer, we’re quickly learning that even people with the same diagnosis will have very different diseases, and may benefit from different therapies. Professor Simon Mitchell and his group have a clear vision: to use computer simulations of individual patient’s disease, to give the right drugs to the right people. They are pioneering these approaches using a combination of computational work, laboratory science, and samples from patients. They are working towards a future where the biopsy used to diagnose blood cancer, will also be used to create a personalised simulation of the disease. The computer simulation can then be used to rapidly predict how the patient will respond to each therapy. Doctors will then use this information when choosing the right treatment for their patients. Recent publications from Dr Mitchell’s team have shown that simulations can predict how different cancer cells will respond to different drugs, laying the foundation for computer-aided personalised treatments in blood cancer.
Their approach is highly interdisciplinary and collaborative as they work closely with experimental science experts such as Professor Chris Pepper and Professor Andrea Pepper, Clinicians such as Dr John Jones, and the Haematology Research Group that includes experts in molecular biology and drug discovery from the University of Sussex.
BACKGROUND IMAGE FOR PANEL
Engaging with patients and the public about new genomic medicine technologies through creative methods

Genomic medicine is an emerging medical discipline that involves using genomic information about an individual as part of their clinical care. Professor Bobbie Farsides and Dr Rich Gorman have been working with patient groups and families affected by rare disease to explore how the promissory discourses surrounding these medical technologies are (re)shaping the social worlds and lived experiences of patients and their families. Their aim has been to use arts-based narratives, co-produced with participants, as a means of creating accessible resources that develop opportunities for public engagement about the lived experience of rare disease, as well as supporting the development of ethically prepared healthcare professionals. The arts-health methods mobilised have provided valuable data. They have also been highly popular with stakeholder groups wishing to encourage public discussions, and Bobbie and Rich’s research has been exhibited at events such as The Festival of Genomics & Biodata, as well as featured on the radio, prompting greater public understanding and dialogue about the arrival of these novel technologies into the clinic.
BACKGROUND IMAGE FOR PANEL
Palliative Care in Advanced Chronic Liver Disease: Time for Action
Advanced chronic liver disease (ACLD) has high morbidity and mortality. Despite this, palliative interventions remain woefully inadequate. Development of fluid in the abdomen (ascites) is the most common complication of ACLD and once refractory to medical treatment the average life expectancy is 6-12 months. Such patients need hospital admission every 10-14 days for drainage. Only a small minority receive a curative treatment such as a liver transplant or a shunt in the liver (TIPS). Professor Sumita Verma and her team are researching a novel intervention (long-term abdominal drain -LTADs). These drains allow drainage of small amounts of fluid guided by patients so can improve symptom control and quality of life. They also allow patients to be managed in their own homes and for them to spend their remaining time outside of hospital. Following on from a feasibility study (REDUCe), Prof Verma and collaborators have received funding for a national 35-site trial to further assesses these LTADs. Both REDUCe and REDUCe 2 studies are funded by the NIHR and run by the Brighton and Sussex Clinical Trials Units. Collaborators include colleagues from Sussex (SHORE-C), Kent, Surrey, Southampton, Exeter, London and a strong PPI group.
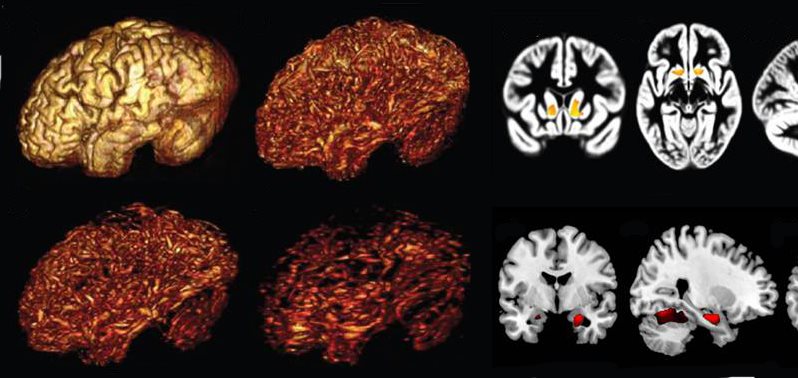
Time for Dementia: enhancing dementia care in the future healthcare workforce

Healthcare for people with dementia is sub-optimal. This is due in part, to a lack of skills and positive attitudes in the healthcare workforce. In 2014, BSMS developed the Time for Dementia (TfD) programme to address this challenge in the future healthcare workforce. As part of the TfD model, students visit a family (person with dementia and their carer) on six occasions over a two-year period, with supporting pedagogic activities. Quantitative evaluation of the programme has shown a higher-level dementia knowledge and attitude change in students who undertook the programme compared with students who did not. Qualitative interviews and focus groups have demonstrated improvements in dementia understanding and attitudes, as well as improved person-centred care to patients with dementia. Due to the positive evaluation findings, TfD has been delivered across 10 different healthcare training programmes at nine higher education institutes across the South of England.
BACKGROUND IMAGE FOR PANEL
Improving healthcare experiences for neurodivergent people
Neurodivergent people face barriers to accessing healthcare. Despite this, in the case of autistic people, we know that life expectancy is reduced and that they live with more co-occurring health conditions. Neurodivergent doctors may be an important piece of the puzzle in improving the healthcare system for the wider neurodivergent community. Over the last decade, research led by Dr Sebastian Shaw at BSMS along with other researchers has been extensively exploring the experiences of neurodivergent people in relation to healthcare – both those of medical students / doctors and those of people accessing healthcare. A key part of this strategy has been centring neurodivergent people within the research, impacting the research and subsequent clinical priorities from the inside. Recently, this work has culminated in the creation of the ‘Autistic SPACE’ framework – guidance for providing real-world adjustments for autistic people in health settings. This framework has now been incorporated into the Royal College of Psychiatrists’ National Autism Training Programme for Psychiatrists (Foundation Course). It has also been incorporated into clinical practice guidelines for GPs through the Scottish National Autism Implementation Team. The Royal College of Speech & Language Therapists have also recently incorporated it as a key resource for providing reasonable adjustments in clinical settings.
BACKGROUND IMAGE FOR PANEL
Controlling institutional scabies outbreaks in care homes for the elderly, refugee camps, and beyond

Scabies is something most of us don’t think about often, and don’t want to think about! It’s caused by a mite that lives in the skin, and is transmitted mainly by close physical contact. In addition to severe distressing itching, it can lead to secondary infections with long-term health impacts. Scabies is most common in the global south, but institutional outbreaks remain a public health problem worldwide (including in the UK) in settings such as care homes for older people, prisons, hospitals, and refugee camps.
At BSMS Jo Middleton and Jackie Cassell have led a unique research programme which has described the problem and generated solutions. This has included (1) providing doctors with new diagnostic criteria for scabies in the elderly, (2) giving recommendations to aid organisations on how to improve management in refugee camps, and (3) championing new treatments for outbreak control. In the first ever National Guidance for scabies outbreaks, most of the research cited is from BSMS.
A new way of managing children’s allergy and asthma

Prof Somnath Mukhopadhyay, together with Dr Elaney Youssef, Dr Tom Ruffles and their research team, have been leading the development of personalised and stratified healthcare within children’s asthma and allergy. Their first-ever randomised clinical trial tested genotype specific treatments for asthma demonstrated improved quality-of-life. Stratified care interventions have become life-changing for the most severely affected asthmatic patients and are benefiting children in Brighton clinics. Their research has changed clinical guidance and media attitudes towards personalised medicine, influenced allergy training by the Royal College of General Practitioners and management guidance from the National Asthma Council in Australia. A programme of NHS-backed clinical PhDs is now seeking to enhance the management of Sussex children through stratified healthcare. New ways of treating asthma are emerging from the identification of a novel children’s asthma and allergy subtype where disease is driven by skin (Brighton, Edinburgh, Berlin). Inclusive research is exploring barriers to introducing personalised medicine within routine allergy-related care in the UK and beyond. Genomics England and genomics implementation programmes in the UAE have expressed interest in discussions to help mainstream children’s allergy health within the “silent revolution” of stratified healthcare.
BACKGROUND IMAGE FOR PANEL
Paradigm changes for trials and treatment in ALS

Amyotrophic Lateral Sclerosis (ALS; also known as Motor Neurone disease, MND) is a fatal neurodegenerative condition for which there is no effective treatment. The MIROCALS (Modifying Immune responses and Outcomes in Amyotrophic Lateral Sclerosis) study co-led by Professor Nigel Leigh (Chief Investigator) represents a major European effort – funded through the EU H2020 programme in partnership with the Motor Neurone Disease Association and other charities- to find an effective treatment to improve survival and quality of life. In a large randomised placebo-controlled trial designed and coordinated by the University Hospital of Nimes in France and BSMS, the MIROCALS study has shown that a low dose of interleukin-2 (IL2) significantly prolongs survival after 18 months treatment. Furthermore, for the first time in ALS trials the study systematically included molecular and cellular biomarkers in blood and cerebrospinal fluid to better understand variations in response to treatment, representing progress towards ‘personalised medicine’ in this devastating disorder. The Consortium coordinators are currently preparing the scientific report for publication and the full study dossier required for regulatory submissions.
BACKGROUND IMAGE FOR PANEL
Developing sustainable models of high-quality healthcare

Climate change poses a major public health threat, and the healthcare sector contributes towards this, responsible for 5% of greenhouse gas emissions. There is growing awareness and momentum towards developing sustainable models of high-quality healthcare, and it is important that an evidence-based approach is taken. The Sustainable Healthcare Group at BSMS, led by Professor Mahmood Bhutta, alongside Dr Chantelle Rizan and Dr Anna Jones and a growing team, are undertaking leading research, education, and shaping policy focusing on mitigating impact of healthcare on the environment, and on related labour rights issues in manufacture of medical goods in low and middle income countries.
The group seek to translate their research into influencing practice and policy; as report chair (Prof Bhutta) and academic chair (Dr Rizan) of a national Green Surgical Care Report in collaboration with the UK Health Alliance on Climate Change, and as senior advisors on an Intercollegiate Green Surgery Checklist. Their work on mitigating the carbon footprint of Personal Protective Equipment featured in a WHO report and informed NHS England policy. They collaborate closely with the Greener NHS, including through Dr Rizan’s Knowledge Exchange Policy Fellowship, and Prof Bhutta serves on a clinical advisory board. Sustainability is reflected in our BSMS20 (20th anniversary) theme, ‘a sustainable and inclusive medical school’, and is a core theme of the Brighton and Sussex Health Research Partnership.
HIV and STI diagnosis and treatment

Timely HIV and STI diagnosis and treatment is a public health priority and relies on accessible testing. Technology-driven approaches, such as the distribution of test kits through vending machines, have the potential to significantly enhance access to testing. For the first time, we implemented vending machines that dispense both STI self-sampling kits and HIV self-test kits in public locations, including libraries, shopping centers, and university campuses in Brighton and Bristol. Our findings demonstrate that the use of these vending machines was both convenient and acceptable, effectively reaching individuals who infrequently or had never previously tested for HIV and STIs.
Vending machines for sexual health are now being used in several countries, including Zambia, Japan, Australia, and Jamaica, to serve different populations. We are now working on the next generation of machines that will dispense reproductive health products such as contraceptives and pre-exposure prophylaxis (PrEP) for HIV prevention.
BACKGROUND IMAGE FOR PANEL
Emerging Innovations in Infection Prevention: Shaping the Future of Global Health
Healthcare-associated infections (HCAIs) and antimicrobial resistance (AMR) present persistent global challenges, causing substantial morbidity, mortality, and economic burden. While traditional approaches focus on controlling infections after they occur, they often fail to address the root causes proactively. Novel technologies, such as whole-genome sequencing (WGS) and artificial intelligence (AI) prediction tools, offer transformative potential by enabling healthcare systems to shift from reactive to preventative infection control, improving patient outcomes, reducing antimicrobial use, and safeguarding the future of global health.
Dr James Price and his research group have made significant contributions to advancing infection prevention and control (IPC) by integrating research, clinical practice, and public engagement. During the COVID-19 pandemic, he developed a real-time surveillance system for hospital-onset infections, which reduced cases by 90% in his Trust and influenced national NHS and WHO guidelines. As a principal investigator within the COVID-19 Genomics UK (COG-UK) Consortium, he demonstrated the value of WGS in informing IPC strategies, shaping international pandemic recovery plans.
Beyond COVID-19 he has pioneered predictive analytics and surveillance frameworks to address AMR and HCAIs, including research challenging existing MRSA prevention hypotheses. His contributions to international guidelines for managing multidrug-resistant organisms have been adopted globally as gold standards, directly impacting patient safety and healthcare efficiency.
His commitment to public engagement has further amplified the impact of his work. Collaborating with internationally recognised bio-artists, Dr Price has co-created exhibitions exploring AMR, reaching over 2.2 million people across the UK, USA, India, and China. These exhibitions have successfully increased public understanding of AMR, with post-event analyses demonstrating enhanced awareness of antimicrobial stewardship and its importance in healthcare sustainability.
Dr Price’s contributions have been recognised through numerous accolades, including the ACCIA National Clinical Impact Award and the European Society for Clinical Microbiology and Infectious Diseases Young Investigator Award. He has secured over £7 million in research funding, authored 90 peer-reviewed publications, and serves as an advisor to national and international health organisations.
Dr Price envisions establishing an internationally recognised academic centre for translational infection research. This centre will focus on:
- Integrating WGS, AI, and predictive analytics into routine clinical practice to pre-emptively combat HCAIs and AMR.
- Developing scalable solutions to align healthcare decarbonisation with robust IPC measures.
- Collaborating with global stakeholders to enhance preparedness and resilience against emerging infectious threats.
In the short term, Dr Price aims to expand WGS and AI-driven IPC tools and foster interdisciplinary partnerships to address healthcare sustainability challenges. Long-term, his goal is to reshape IPC research and clinical practice, reducing the global burden of HCAIs and AMR while creating a safer, more sustainable healthcare system.
Dr Price’s work exemplifies how innovation in research, clinical practice, and public engagement can transform IPC, leaving a lasting impact on healthcare systems worldwide.
BACKGROUND IMAGE FOR PANEL
Emerging impact: Evaluating the impact of tobacco control policies
Tobacco smoking is the leading cause of preventable death globally, killing over 8 million people each year including over 1 million from second-hand smoking. Smoking also remains a leading cause of inequity—it causes at least 50% of the difference in life expectancy between the least and most deprived in England.
At BSMS, Dr Katie East leads the England arm of the International Tobacco Control (ITC) Policy Evaluation Project to evaluate the impact of tobacco control policies on driving down smoking prevalence.The ITC Project is the first ever international cohort study of tobacco use. Its overall objective is to measure the psychosocial and behavioural impact of key national level policies of the WHO Framework Convention on Tobacco Control (FCTC). This objective is achieved through analysing longitudinal cohort survey (with replenishment) of adults who smoke in multiple countries (including England). Findings from one country can then be used to inform policies in other countries. Further information is available at itcproject.org.
The work that Dr Katie East has been involved in has found that policies like banning menthol in cigarettes, increasing the age of sale, standardising packaging, and banning smoking in public places have changed smoking behaviours and attitudes. For example, in England before menthol was banned in cigarettes, around 12% of youth who smoked in England smoked menthol cigarettes; however, after the menthol ban this number dropped to 3%. This decrease was also greater than changes observed in Canada and the US, where menthol cigarette policies remained unchanged during the study period. Thus, there is strong evidence that England’s menthol cigarette ban reduced menthol smoking among youth.
Findings from the ITC Project have been used to inform policy globally. For example, the ITC work on banning menthol in cigarettes was used as evidence by the US FDA to inform their proposed rule to ban menthol in cigarettes. ITC evidence on increasing the age of sale was used to inform the ‘smokefree generation’ as part of the UK 2024-25 Tobacco and Vapes Bill. Dr East has also written sections for the 2024 Royal College of Physicians report on E-Cigarettes and Harm Reduction and the 2022 Office for Health Improvement and Disparities Nicotine Vaping in England report, drawing on ITC evidence.
Dr East has also spoken about her work using ITC data to TIME magazine, the Department of Health and Social Care, the Office for Health Improvement and Disparities, Cancer Research UK, the Royal College of Physicians, Action on Smoking and Health, the Public Health Research Consortium, Health Canada, and the Canadian Public Health Association.
Emerging impact: Implementation preferences for the management of sexually transmitted infections in the South African health system: a discrete choice experiment

Sexually transmitted infections (STIs) have historically been neglected within South Africa’s National Sexual and Reproductive Health (SRH) programme. Recognising this gap, there is renewed political will and a strategic focus on transitioning from syndromic STI management to an aetiology-based approach. This shift aims to integrate STI care into a comprehensive service that seamlessly incorporates SRH and HIV prevention. Achieving this vision requires a systems-based approach that ensures health system readiness, builds in-country capacity for STI-focused and related research, trains healthcare providers (HCPs), and supports clinical mentors and implementers within the National Department of Health (NDOH) to drive policy execution.
The South African National Strategic Plan (NSP) 2017–2022 highlights key priorities, including the evaluation of digital and point-of-care (POC) technologies for STI care delivery. The HIV pre-exposure prophylaxis (PrEP) programme is rapidly expanding, with approximately 1.34 million people initiated on PrEP by November 2024. Despite this progress and the willingness to adopt an aetiology-based approach for STI management, evidence on effectively integrating this model within the PrEP programme remains scarce.
To address this gap, we conducted a discrete choice experiment to investigate primary care service users’ preferences for STI diagnosis and treatment in South Africa. The findings revealed that most service users (68%) preferred to undergo STI testing before treatment, self-collect samples for testing, and receive same-day treatment. Expedited partner notification was also favoured by the majority of participants. The availability of POC STI technologies, capable of delivering results within 30 minutes, aligns with the care model preferred by participants, making it a feasible option. However, implementation within real-world clinical settings requires further evaluation.
Our study was recognised by the World Health Organization (WHO) as a case study in its guidance document, WHO Implementation Tool for PrEP of HIV Infection – Integrating STI Services.
BACKGROUND IMAGE FOR PANEL
Emerging impact: Consultation, Campaign and Medication: Changing public understanding of scabies outbreak in Rwanda, Sudan and Ethiopia amongst fragile population in refugee camps and those internally displaced

Scabies is found across the globe but is most common in tropical areas and affects communities already disadvantaged by poverty, overcrowding or conflict. It is highly contagious with a debilitating parasitic infection having a significant impact on the quality of life. The condition is targeted for control by WHO, which encourages countries to incorporate scabies management into their universal health coverage package of care. Research led by Professor Gail Davey and her NIHR-funded 5S research team have been engaging with scabies affected communities in Ethiopia, Rwanda and Sudan, who are already disadvantaged by poverty, overcrowding or conflict and “hard-to-access” groups to raise awareness and early detection of the condition in Internally Displaced Peoples (IDP) camps. The public awareness raising campaign is providing new knowledge and skills to control the spread of scabies and has impacted on the practices, customs and attitudes of individuals in the camps. In Sudan, a week-long campaign supported by El Gezira University and the Ministry of Health enabled identification, treatment and demystification of scabies in this highly vulnerable population. As well as public awareness-raising, over 600 people underwent medical check-ups with a dermatologist, identifying 494 people suffering from scabies. Over 8500 individuals were reached through these campaigns. Medication was distributed, and further supplies left with the medical centres at the IDP camps. The work of the Global Health Research Unit (BSMS) and the 5S Foundation working closely with local stakeholders is beginning to transform the lives of fragile communities, the latter live in fear of the disease and find contracting scabies as highly shameful. Furthermore, diagnosis and availability of medication is beginning to transform awareness of the condition and in turn communities’ response to scabies.
BACKGROUND IMAGE FOR PANEL
Emerging impact: Building the dementia workforce of the future

Healthcare for people with dementia in the 21st century is sub-optimal. This is due, in part to a lack of skills and positive attitudes in the healthcare workforce. In 2014, BSMS developed the Time for Dementia programme to address this challenge in the future healthcare workforce. As part of the Time for Dementia model, students visit a family (person with dementia and their carer) on six occasions over a two-year period, with supporting pedagogic activities. Our research has shown a higher level of dementia knowledge and attitude change in students who have undertaken the programme compared with students who did not. Qualitative research has demonstrated improvements in dementia understanding and attitudes as well as improved person-centred care to patients with dementia. These positive findings have led to the expansion of Time for Dementia across 10 different healthcare training programmes at 11 universities across the United Kingdom. Ongoing Time for Dementia research is seeking to assess the impact of learning into clinical practice.
Find out more about Time for Dementia here >
Emerging Impact: elevated blood pressure and hypertension

Prof Richard McManus was a member of the European Society of Cardiology Guideline Development Group for the 2024 Guidelines on the management of elevated blood pressure and hypertension. These guidelines were developed over a two year period and introduced several new evidence based concepts, in particular regarding the continuum of risk for high blood pressure and the importance of out-of-office BP measurement in the management of hypertension. Blood pressure levels are reframed as “non-elevated BP,” “elevated BP,” and “hypertension.” And treatment for those at highest risk is now recommended down to a target of 120-129 systolic blood pressure, provided it is well tolerated. Self and ambulatory BP monitoring are recommended for both diagnosis and management. More details can be found here.
This contribution highlights a clear example of clinical and policy impact, with research evidence directly shaping international guidelines that influence everyday clinical practice across Europe and beyond. It builds on guidelines from NICE and in the US which respectively led changes towards out of office measurement and to reduce treatment targets based on cardiovascular risk. The new BP classifications and treatment thresholds are expected to improve earlier identification of at-risk patients, support personalised treatment decisions, and ultimately reduce preventable strokes and cardiovascular events. The explicit endorsement of self-monitoring demonstrates how academic findings from research, including that undertaken in the UK by Richard’s group, translate into better tools for patients and clinicians. With >1.3m downloads and >750 citations already, the guidelines have shown rapid academic uptake, but more importantly they are now being embedded into health systems, professional training, and patient care pathways worldwide. This illustrates how sustained research engagement can deliver tangible outcomes in both healthcare, while strengthening the UK’s role in setting international standards.
BACKGROUND IMAGE FOR PANEL
Long-acting HIV treatment included in WHO treatment guidelines

Long-acting injectable HIV treatment represents a transformative shift in therapeutics and could be pivotal in ending the global HIV epidemic. Dr Fiona Cresswell recently served as a site Principal Investigator in a multicountry clinical trial (Cabotegravir and Rilpivirine Efficacy and Safety Study, CARES, published in The Lancet Infectious Diseases), the evidence from which has directly influenced and reshaped WHO guidelines. WHO announced the inclusion of injectable treatment in their global HIV treatment guidelines at the International AIDS Society Conference (IAS) in Kigali in July 2025. The results of a second phase 3 trial led by Fiona Cresswell were also featured at the IAS conference this year, further consolidating the evidence base for long-acting therapy. Three PhD students at BSMS are currently working on generating more data on drug resistance, metabolic outcomes, and interactions with hepatitis B virus, thereby expanding the understanding of long-acting HIV treatment’s global impact.
BACKGROUND IMAGE FOR PANEL
Uncovering the immune mechanisms behind podoconiosis

Led by Professor Mel Newport and Dr Fisal Tantoush, this MRC-funded project worth more than £1million funding seeks to transform the way we understand and manage podoconiosis, a neglected tropical disease (NTD), through a fourfold impactful vision: eliminating the disease, advancing immunological science, introducing ‘-omics’ and single-cell technologies to Ethiopia, and expanding genomic data for African populations. A strategic partnership between BSMS, Armauer Hansen Research Institute, Arba Minch University and the Wellcome Sanger Institute will drive this vision forward. By applying single-cell transcriptomics to podoconiosis, the research could lead to a novel diagnostic test and inform WHO guidelines for NTDs. Beyond podoconiosis, the project has broader implications for other HLA-associated, environmentally triggered inflammatory diseases. It also addresses global inequities in genomic research by building local capacity in Ethiopia, including training early-career researchers and fostering long-term institutional collaboration. The work is embedded in a multidisciplinary network, ensuring social and economic impact through integration with ethics, development economics and behavioural science. Beneficiaries include patients, communities, researchers, health workers and policymakers, with potential for future commercial collaboration if a molecular signature is identified.
Advancing Tuberculous Meningitis Treatment in LMICs

TB meningitis is a disease that is prevalent in Low- and Middle-Income Countries and is frequently fatal or leaves survivors with life-altering disabilities. Dr Fiona Cresswell, along with a multinational research team in Uganda, Indonesia, South Africa, the Netherlands and USA, has recently completed the first phase 3 clinical trial to include both African and Asian adults with TB meningitis, marking a critical advance in global TB research. The trial examined the impact of high-dose rifampicin on TB meningitis outcomes. The results were presented at the European Society of Clinical Microbiology and Infectious Diseases in Vienna in April 2025 and will be published in the New England Journal of Medicine later this year, positioning this study to shape future treatment research direction.
BACKGROUND IMAGE FOR PANEL
Laying the Foundations for Community-Led Hearing Care

The November 2025 visit by Prof Mahmood Bhutta and Dr Alan Sanderson to Malawi and Zambia marked the formal launch of the NIHR Global Health Research programme on community-based ear and hearing care for people living with chronic suppurative otitis media (CSOM). This visit represents a critical early impact milestone, establishing the foundations required for sustained scientific, health system, and community-level impact over the life of the programme and beyond.
Emerging impact includes the successful establishment of four interconnected work packages—lived experience, treatment, hearing rehabilitation, and Deaf empowerment which together provide a coherent, community-centred framework for addressing CSOM. Through meetings at the Malawi–Liverpool–Wellcome Programme (MLW) and ZAMBART, the team co-developed locally appropriate research systems with clinicians, academics, community engagement specialists, and professionals in translation, transcription, and data management. These collaborations ensure that the research is scientifically rigorous, culturally embedded, and responsive to community priorities from the outset.
A key early impact is capacity strengthening. The programme has recruited and engaged PhD students based in Malawi, Zambia, and Cambodia, who will lead in-country data collection and analysis. This investment builds sustainable research leadership in low- and middle-income countries (LMICs) and supports long-term ownership of evidence generation, policy translation, and service development.
Looking ahead, the programme aims to empower communities by evaluating and supporting low-cost, scalable interventions such as iodine-based treatments and affordable hearing devices that can be safely adopted at community level without reliance on specialist health professionals. By generating transferable evidence with relevance beyond the study countries, the research has the potential to benefit the estimated 300 million people worldwide living with CSOM, extending its impact well beyond the immediate settings of the programme.